- Home
-
Screening
- Ionic Screening Service
-
Ionic Screening Panel
- Ligand Gated Ion Channels
- Glycine Receptors
- 5-HT Receptors3
- Nicotinic Acetylcholine Receptors
- Ionotropic Glutamate-gated Receptors
- GABAa Receptors
- Cystic Fibrosis Transmembrane Conductance Regulators (CFTR)
- ATP gated P2X Channels
- Voltage-Gated Ion Channels
- Calcium Channels
- Chloride Channels
- Potassium Channels
- Sodium Channels
- ASICs
- TRP Channels
- Other Ion Channels
- Stable Cell Lines
- Cardiology
- Neurology
- Ophthalmology
-
Platform
-
Experiment Systems
- Xenopus Oocyte Screening Model
- Acute Isolated Cardiomyocytes
- Acute Dissociated Neurons
- Primary Cultured Neurons
- Cultured Neuronal Cell Lines
- iPSC-derived Cardiomyocytes/Neurons
- Acute/Cultured Organotypic Brain Slices
- Oxygen Glucose Deprivation Model
- 3D Cell Culture
- iPSC-derived Neurons
- Isolation and culture of neural stem/progenitor cells
- Animal Models
- Techinques
- Resource
- Equipment
-
Experiment Systems
- Order
- Careers
Cerebral-Spinal Injury Model
Cerebral-Spinal Injury includes both Traumatic Brain Injury (TBI) and Spinal Cord Injury.
Traumatic brain injury (TBI)
As a leading cause of death and disability for people under the age of 45 years, TBI is defined as damage to the brain resulting from an external mechanical force, such as caused by rapid acceleration or deceleration, blast waves, crush, an impact or penetration by a projectile. TBI can lead to temporary or permanent impairment of brain functions including: cognitive, physical and psychosocial functions.
TBI affects millions of individuals worldwide. In 2010 alone, the United States Centers for Disease Control reported 2.5 million TBI's nationwide. TBI's are heterogeneous injuries that can range from an apparently “mild” concussive impact with no clear damage, to penetrating head traumas with obvious wide-spread tissue loss.
Multiple TBI animal models are available in Creative Bioarray. For example, we conduct the controlled cortical impact (CCI) model of traumatic brain injury to evaluate preclinical therapies. CCI is a widely-used and well-characterized model which produces clear motor and cognitive deficits and may be ameliorated with pharmacotherapies such as progesterone.
Common outcome measurements include:
Beam balance motor test
Cognitive performance: Morris Water Maze
Gait analysis
Acute edema in the brain
Histological measures such as the cortical lesion volume.
For a comprehensive evaluation of injury location, severity, and multiple occurrences of TBI, Creative Bioarray continuously develops novel TBI models for therapeutic compounds evaluations. In Creative Bioarray, all studies can be customized and adjusted to fit client needs. Our traumatic brain injury work takes both short-term recovery and treatments as well as longer-term functional and cognitive outcomes into account. Acute or long-term (chronic) histological, functional and behavioral follow-up are both available. In addition, we leverage our extensive MRI/MRS capability to provide comprehensive studies with superior quality as well as a more comprehensive data package generated from the models.
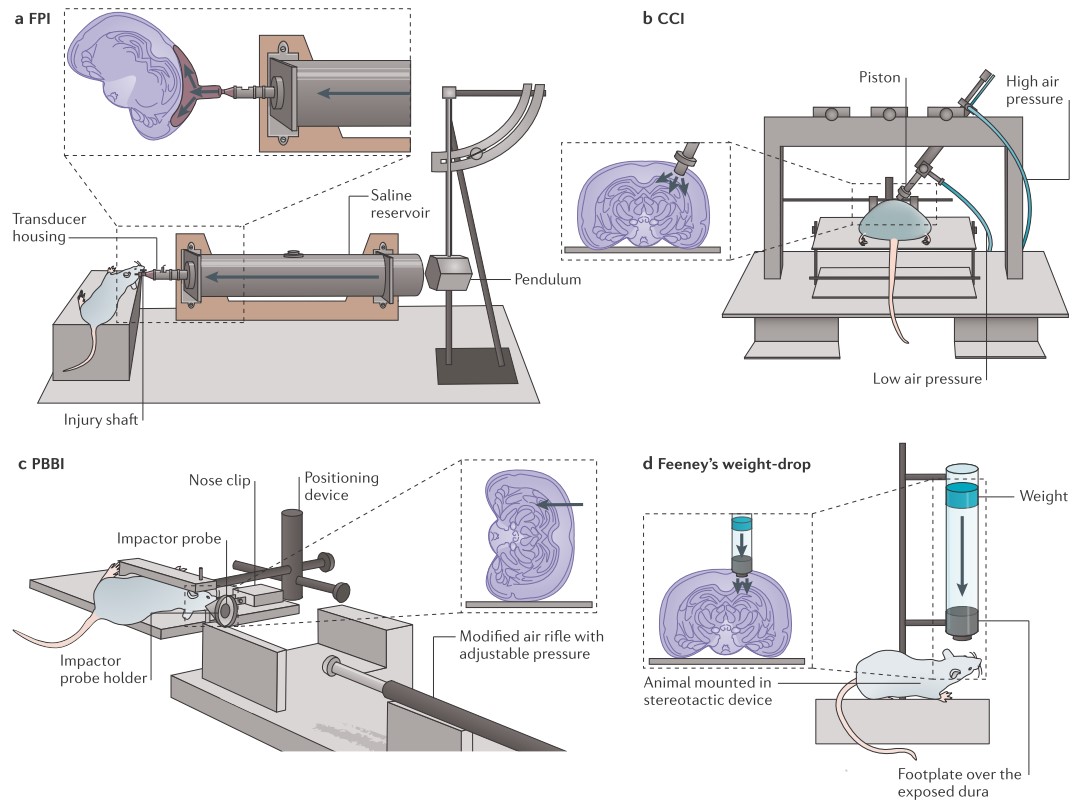
Fig. 1 Experimental set-ups for the animal models of TBI
Spinal Cord Injury (SCI)
In recent years, there have been numerous reports of interventions that enhance sparing of function and/or promote repair mechanisms including axon regeneration so as to enhance recovery of function after SCI. While, there remains no clinical cure for SCI which can result in devastating functional deficits such as complete paralysis.
A barrier to translation is that there are often no published replications of promising studies, raising questions about reproducibility. To address this, stable SCI models are in need. Creative Bioarray has constructed multiple established animal models of spinal cord injury to test the efficacy of novel therapeutics. Creative Bioarray utilizes the model of thoracic SCI which produces a spinal cord contusion with a precisely controlled impact force. This spinal cord contusion mimics the contusion injuries which frequently occur in human SCI. SCI animals exhibit hind limb paralysis which can progressively recover over the ensuing weeks following injury.
Common outcome tests include:
Basso-Beattie-Bresnahan (BBB) locomotor rating scale
Foot faults in the horizontal ladder test
Gait analysis
Histological measurements such as the lesion size and white matter sparing
Models of SCI
Mild/Moderate T10 contusion injury
Severe T10 contusion injury
Hemi-section model (unilateral injury)
Creative Bioarray helps researchers look at short-term histological changes as well as long-term and more comprehensive outcomes within an extensive functional battery. We offer powerful tools to evaluate elements of neuro-protection and neuro-regeneration.
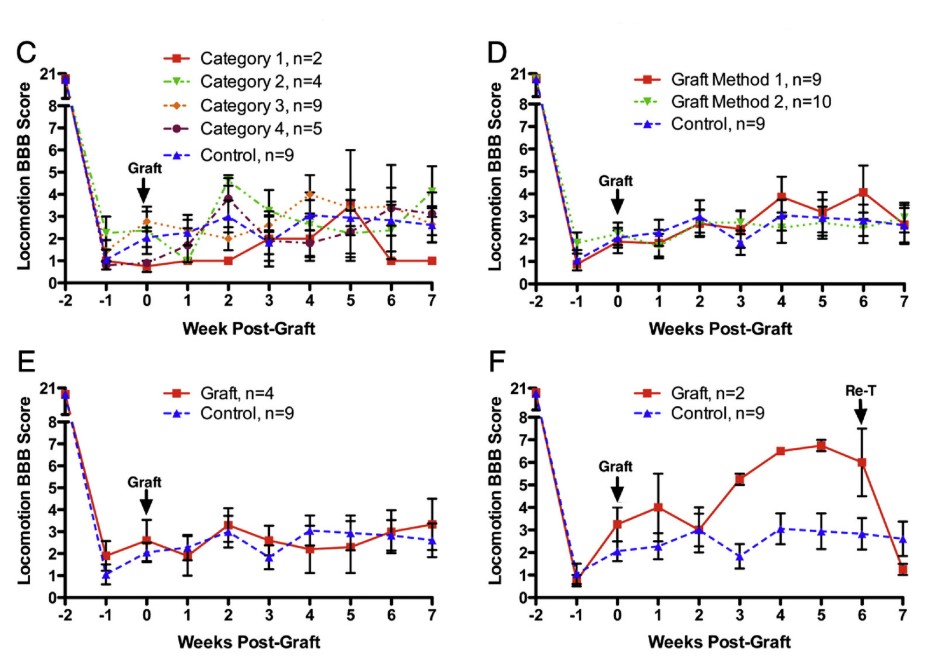
Fig.2 Functional assessments: Comparison of data from rats with different categories of transplants or using different Methods by BBB scores analysis
References
Xiong Y, et al. Animal models of traumatic brain injury. Nat Rev Neurosci. 2013; 14: 128–142.
Sharp KG, et al. A re-assessment of long distance growth and connectivity of neural stem cells after severe spinal cord injury. Exp Neurol. 2014; 257: 186–204.
Related Section
- Alzheimer's Disease Model
- Parkinson's Disease Model
- Huntington's Disease Model
- Epilepsy Model
- ALS Model
- Psychiatric Model
- Autism Spectrum Disorder
- Pain Model
- Stroke Model
- Fragile X Model
- Acute/Chronic Heart Failure Model
Inquiry

