- Home
-
Screening
- Ionic Screening Service
-
Ionic Screening Panel
- Ligand Gated Ion Channels
- Glycine Receptors
- 5-HT Receptors3
- Nicotinic Acetylcholine Receptors
- Ionotropic Glutamate-gated Receptors
- GABAa Receptors
- Cystic Fibrosis Transmembrane Conductance Regulators (CFTR)
- ATP gated P2X Channels
- Voltage-Gated Ion Channels
- Calcium Channels
- Chloride Channels
- Potassium Channels
- Sodium Channels
- ASICs
- TRP Channels
- Other Ion Channels
- Stable Cell Lines
- Cardiology
- Neurology
- Ophthalmology
-
Platform
-
Experiment Systems
- Xenopus Oocyte Screening Model
- Acute Isolated Cardiomyocytes
- Acute Dissociated Neurons
- Primary Cultured Neurons
- Cultured Neuronal Cell Lines
- iPSC-derived Cardiomyocytes/Neurons
- Acute/Cultured Organotypic Brain Slices
- Oxygen Glucose Deprivation Model
- 3D Cell Culture
- iPSC-derived Neurons
- Isolation and culture of neural stem/progenitor cells
- Animal Models
- Techinques
- Resource
- Equipment
-
Experiment Systems
- Order
- Careers
Familial Atrial Fibrillation
Atrial fibrillation is one of the most common clinical tachyarrhythmias. With the aging of the social population, the incidence of atrial fibrillation is gradually increasing. Its serious complications include cerebral embolism, stroke, etc., and stroke is also an important factor in death from atrial fibrillation. In recent years, significant progress has been made in the pathogenesis of atrial fibrillation, and the understanding of atrial fibrillation from the aspects of genes and ion channels has been fully updated. The application of new genetic research methods to reveal the mechanism of gene mutations leading to some familial atrial fibrillation, which helps to understand the molecular mechanism of atrial fibrillation and the resulting electrophysiological changes.
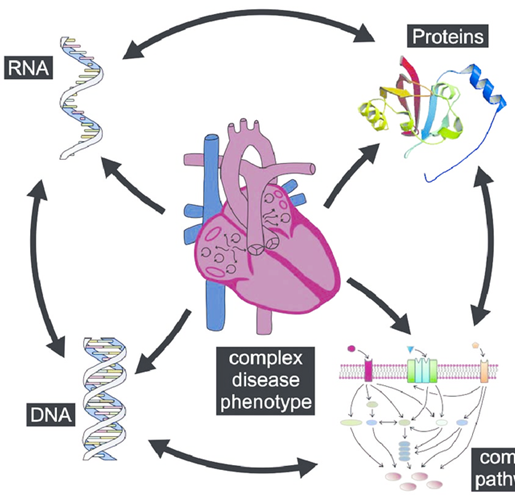
Figure 1. Schematic illustration of atrial fibrillation (AF) pathophysiology. (Moritz F Sinner, et al.; 2011)
Genetic Characteristics of Familial Atrial Fibrillation
The inheritance pattern of familial atrial fibrillation accords with Mendelian inheritance pattern. In 1943, Wolff reported that the occurrence of atrial fibrillation was related to vagus nerve hypertonia, and reported single-gene familial atrial fibrillation. In 1963, Phair also mentioned that hypertonic vagus nerve may be the cause of atrial fibrillation. In 1996, Brugada et al. conducted a study on the genetic location of familial atrial fibrillation, and located the atrial fibrillation gene on chromosome 10, which was autosomal dominant. According to clinical practice, Dar-bar et al. found that 5% of patients with typical atrial fibrillation and 15% of patients with solitary atrial fibrillation were hereditary, indicating that familial atrial fibrillation is not as rare as before. The four families of atrial fibrillation they studied all eliminated the previously discovered familial atrial fibrillation gene locus related to chromosome 10 10q22-q24, and finally concluded that familial atrial fibrillation is a genetically heterogeneous disease. At least two pathogenic genes are related to familial atrial fibrillation. Interestingly, in addition to chromatic inheritance, clinical genetic analysis found that atrial fibrillation also has X-linked dominant inheritance.
Molecular Mechanism of Disease
Since Brugada et al. found genes that can cause atrial fibrillation in 1996, at least 10 mutagenic genes have been discovered so far. Familial atrial fibrillation is the same as other familial diseases and has genetic heterogeneity. Even if the pathogenic genes are the same, the pathogenic mutations are often different.
Familial atrial fibrillation and potassium channel gene mutation
In 2003, Chen et al. used human genome-wide microsatellite molecular markers (SSR) to discover and identify the S140G mutation in the KCNQ1 gene at chromosome 11p15.5 in a study of Chinese atrial fibrillation families including four generations of relatives. This point mutation is a missense Mutation, adenine at position 418 of the normal gene is changed to guanine, and serine at position 140 of the corresponding potassium ion channel is changed to glycine. Further studies have found that the modified mutant has an "acquisition function" effect on the KCNQ1/KCNE1 and KCNQ1/KCNE2 currents, that is, when the mutant gene and KCNE1 gene are jointly expressed, it can cause the inward potassium current to increase during hyperpolarization, leading to the action potential time limit and effectiveness The refractory period is shortened. Yang et al. found in 2004 that the onset of atrial fibrillation in two different families was related to the KCNE2 gene R27C mutation. The KCNE2 gene is located on chromosome 21q22. When the mutation of this gene is co-expressed with the KCNQ1 gene, it can cause gains in potassium channel function. KCNE2 encoding Mink homologous protein may be a subunit that rapidly activates delayed rectifier potassium channels and KCNQ1/KCNE2 channels. Mutations in this subunit will produce a background potassium current, which in turn can lead to a shorter action potential time. Clinical studies have shown that the slowly activating potassium current (IKS) composed of α subunit (KvLQ-T1) and β subunit (mink) participates in the atrial muscle phase III repolarization activity. In the study of dog atrial fibrillation model, the use of IKS blocker can terminate the atrial fibrillation of dog atrial fibrillation model, indicating that IKS participates in the pathophysiological process of atrial fibrillation through its β subunit. In addition, in 2006, Darbar et al. discovered a new pathogenic gene KCNA5 in a family line of early-onset isolated atrial fibrillation. This gene is located on chromosome 12p13. The mutation of this gene can affect proline-rich tyrosine kinase for the regulation of the ultrarapid outward current I (IKur), and then leading to a decrease in IKur and a tolerance to tyrosine kinases. These studies indicate that abnormal cardiac potassium channels may be the mechanism that causes atrial fibrillation.
Familial Atrial Fibrillation And Sodium Channel Gene Mutation
The SCN5A gene, located on chromosome 3p21, encodes the Na1.5 channel alpha subunit. The first SCN5A mutation site found to be associated with atrial fibrillation is Asn1986Lys. Further research found that the SCN5A variant is a comprehensive heterozygous variant, such as the original RH1632 and the new variant M858L were found in a patient with familial atrial fibrillation. Researchers believe that individuals who have old and new mutations are more obvious. For example, they have spontaneous atrial arrhythmia in their youth, and gene mutations lead to hyperpolarization transitions that cause cell action potential steady-state inactivation. This change may be related to the early post-depolarization of the delayed atrial action potential period, and this post-depolarization is prone to atrial fibrillation through the conduction bundle in the atrium. It was recently discovered that SCN5A gene variants also include R1860G and N1986K. In addition, studies on the N1986K mutation in Xenopus eggs found that the mutation can produce hyperpolarization and inactivate sodium channels. In addition to cardiac potassium channels participating in the mechanism of atrial fibrillation, cardiac sodium channels are also related to the occurrence of atrial fibrillation.
In addition, non-ion channel gene mutations can also cause atrial fibrillation, such as gap junction gene mutations and ANP gene mutations.
References
- Darbar D, et al.; Familial atrial fibrillation is agenetically heterofeneous disorder. J Am Coll Cardiol. 2003, 41(12): 2185-2192.
- Chen YH, et al.; KCNQ1 gain of function mutation in familial atrial fibrillation. Science. 2003, 229( 5604): 251-254.
- Robyns T, et al.; Reduced penetrance and variable expression of sCN5A mutations and the importance of co-inherited genetic variants: case report and review of the literature. Indian Pacing Electrophysiol J. 2014, 14( 3):133-149.
- Moritz F Sinner, et al.; Recent advances in the genetics of atrial fibrillation: from rare and common genetic variants to microRNA signaling. Cardiogenetics. 2011, DOI: 10.4081/cardiogenetics.2011.s1.e7
Related Section
Inquiry

