- Home
-
Screening
- Ionic Screening Service
-
Ionic Screening Panel
- Ligand Gated Ion Channels
- Glycine Receptors
- 5-HT Receptors3
- Nicotinic Acetylcholine Receptors
- Ionotropic Glutamate-gated Receptors
- GABAa Receptors
- Cystic Fibrosis Transmembrane Conductance Regulators (CFTR)
- ATP gated P2X Channels
- Voltage-Gated Ion Channels
- Calcium Channels
- Chloride Channels
- Potassium Channels
- Sodium Channels
- ASICs
- TRP Channels
- Other Ion Channels
- Stable Cell Lines
- Cardiology
- Neurology
- Ophthalmology
-
Platform
-
Experiment Systems
- Xenopus Oocyte Screening Model
- Acute Isolated Cardiomyocytes
- Acute Dissociated Neurons
- Primary Cultured Neurons
- Cultured Neuronal Cell Lines
- iPSC-derived Cardiomyocytes/Neurons
- Acute/Cultured Organotypic Brain Slices
- Oxygen Glucose Deprivation Model
- 3D Cell Culture
- iPSC-derived Neurons
- Isolation and culture of neural stem/progenitor cells
- Animal Models
- Techinques
- Resource
- Equipment
-
Experiment Systems
- Order
- Careers
- Home
- Symbol Search
| Catalog | Product Name | Gene Name | Species | Morphology | Price |
|---|---|---|---|---|---|
| ACC-RI0112 | Human KCNN4 Stable Cell Line-CHO | KCNN4 | Human | Epithelial-like | INQUIRY |
KCa3.1, the medium-conductance calcium-activated potassium channel, is a member of the calcium-activated potassium channel family. It is activated due to the high level of intracellular Ca2+, which can promote K + efflux, thereby regulating cell membrane potential and intracellular calcium signal. KCa3.1 was cloned by 3 research groups in 1997. The gene encoding KCa3.1 is KCNN4, which is located on chromosome 19 (19 q13.2), and consists of a homotetramer composed of a functional KCa3.1 channel protein; KCa3.1 channel has 6 spans membrane regions in structure, the fifth and sixth transmembrane regions contain K+ selective amino acid sequences, which make them highly selective for K+. The N-terminal of the cell contains an endoplasmic memory signal, which plays a role in the material packaging and transport functions in the cell; the C-terminal of the cell is connected to calmodulin, which is a Ca2+ sensor, which senses the concentration of calcium ions in the cell and Perform regulation.
Physiological Effects of KCa3.1
KCa3.1 is widely distributed in the body, in hematopoietic cells (red blood cells, platelets, lymphocytes, monocytes/macrophages, mast cells), epithelial tissues (stomach, intestine, lung, endocrine glands, exocrine glands), vascular endothelium Cells, fibroblasts, and vascular smooth muscle cells are all distributed. The main physiological effects of KCa3.1: (1) K+ efflux after the KCa3.1 channel is opened, accompanied by cell water loss, which causes red blood cells to dehydrate and shrink; (2) KCa3.1 channels play a role in the activation, migration, and metastasis of lymphocytes, monocytes, macrophages, vascular smooth muscle cells, mast cells and other inflammatory cells; (3) The opening of KCa3.1 channels promotes a variety of cells such as fibroblasts. The proliferation of cells, vascular smooth muscle cells, and vascular endothelial cells; (4) The opening of KCa3.1 channels promotes the transport of water and chloride by epithelial cells, and promotes the secretion of insulin by pancreatic β cells; (5) together with KCa2.3 in vascular endothelial ultra It plays a role in the initiation of the polarizing factor response, causing smooth muscle relaxation.
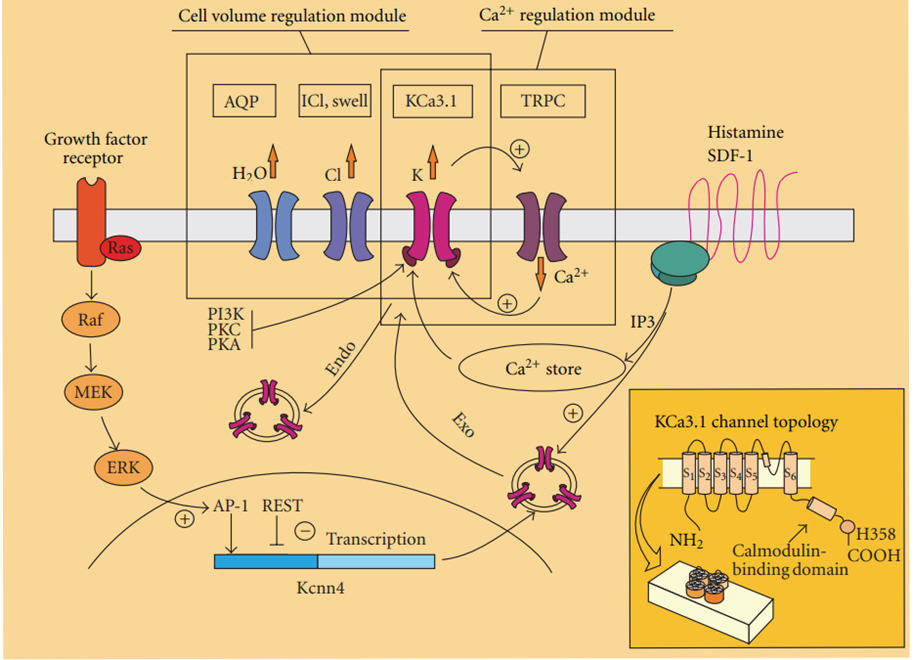
Figure 1. Expression and Role of the Intermediate-Conductance Calcium-Activated Potassium Channel KCa3.1 in Glioblastoma.(Catacuzzeno, et al.; 2012)
KCa3.1 and Related Diseases
Sickle Cell Anemia
Sickle cell anemia is an autosomal dominant hemolytic disease. The sixth amino acid glutamic acid at the N-terminus of the β subunit of the patient's hemoglobin is replaced by valine to form sickle hemoglobin S, which replaces the normal hemoglobin A. Sickle hemoglobin S polymerizes under certain conditions, causing the loss of water and K+ in red blood cells, increasing the density of red blood cells and dissolving. The opening of KCa3.1 channels on red blood cells plays an important role in K+ outflow and water loss. After KCa3.1 channels are blocked, red blood cell lysis is reduced, and the number of high-density red blood cells is reduced, which has a certain protective effect on red blood cells.
Inflammation and Autoimmune Diseases
Most inflammatory and autoimmune diseases are manifested by excessive or delayed inflammatory immune response. Studies have found that KCa3.1 is on vascular endothelial cells, fibroblasts, smooth muscle cells, macrophages, T cells, B cells and other inflammatory cells Both are expressed. And KCa3.1 plays an important role in the proliferation of T cells, B cells, fibroblasts and smooth muscle cells, and the migration of smooth muscle cells and macrophages. It is reported in the literature that the combined application of KCa3.1 blocker TRAM-34 and Kv1.3 blocker ShK can reduce the infiltration of T cells and macrophages in the early stage of renal transplant rejection in rats. Bronchial asthma is a chronic airway inflammatory response involving a variety of inflammatory cells. The anti-asthma effect of KCa3.1 blocker Senicapoc is obvious in asthma sheep model. Acting on the mouse model of autoimmune encephalomyelitis, although the KCa3.1 blocker TRAM-34 cannot reduce the number of T cells infiltrated in the spinal cord, it can significantly reduce the inflammatory response and improve symptoms.
Proliferative Disease
The KCa3.1 blocker TRAM-34 has been proven to reduce postoperative proliferation and restenosis in animal models of coronary artery balloon angioplasty, and its mechanism is mainly to inhibit the phenotypic transition and proliferation of smooth muscle cells. Atherosclerosis is a chronic vascular inflammation and proliferative disease. Its formation involves a variety of cells, including smooth muscle cells, macrophages, T cells and so on. KCa3.1 is expressed on these cells and participates in cellular processes. Application of KCa3.1 blockers can prevent the progression of the disease. It is reported in the literature that drug blocking or gene knockout of KCa3.1 channel can inhibit the proliferation of fibroblasts and reduce renal fibrosis caused by bilateral ureteral obstruction. KCa3.1 channel may become a therapeutic target forchronic kidneys caused by hypertension and diabetes. Idiopathic pulmonary fibrosis is a disease of unknown cause, characterized by diffuse alveolitis and alveolar structural disorders that eventually lead to pulmonary interstitial fibrosis. Myofibroblasts play an important role in the pathogenesis of idiopathic pulmonary fibrosis, and KCa3.1 is highly expressed on myofibroblasts, and participates in their proliferation and fibrosis-promoting function, and may be a treatment target for idiopathic pulmonary fibrosis. In addition, it has been found that KCa3.1 is expressed in a variety of tumor cells such as prostate cancer, leukemia, malignant glioma, breast cancer, pancreatic cancer, endometrial cancer, and melanoma lung metastasis, and participates in the progression of the disease.
Secretion Related Diseases
Polycystic kidney disease is an autosomal dominant genetic disease, characterized by a large amount of fluid in the capsule. The main mechanism of pathogenesis is the outflow of Cl- through epithelial cells. The opening of KCa3.1 channel provides it with potential energy, blocking the channel and significantly improving Condition.
Arterial Vasodilation Disorders
Under the stimulation of acetylcholine, bradykinin, etc. and when hemodynamic changes, vascular endothelial cells produce EDHF, nitric oxide and prostaglandins, three main vasodilator factors. KCa3.1 and KCa2.3 are in the initiation of the EDHF response Play an important role, can hyperpolarize subendothelial smooth muscle cells, close voltage-gated calcium channels, reduce intracellular calcium ion concentration, and relax blood vessels. The rat model of chronic renal insufficiency also showed symptoms of down-regulation of carotid KCa3.1 expression, decreased function, and weakened EDHF response.
References
- Fanger CM. et al.; Calmodulin mediates calcium-dependent activation of the inte rmediate conductance KCa channel, IKCa1. J Biol Chem. 1999, 274(9) :5746-5754.
- Ataga KI, et al.; Effiacy and safety of the Gardos cha nnel blocker seniapoc ( ICA-17043 ). in patients with sickle cell anemia. Hood. 2008,111(8) :3991-3997.
- Grgice I, et al.; Hockade of T-lymphoeyte KCa 3. 1 and Ku 1.3 channels as novel immunosuppression strategy to prevent kidney allograft rejection. Transplant Proc. 2009, 41(6): 2601-2606.
- Chen YJ, et al.; The KCa 3.1 blocker TRAM-34 reduces infarction and neurological deficit in a rat model of ischemia/reperfusion stroke. J Cereb Hlood Flow Metab. 2011, 31(12) :2363-2374.
- Grgic I, et al.; Renal fibrosis is attenuated by targeted disruption of KCa3.1 potassium channeb. Proc Natl Acad Sai USA. 2009, 10(34):14518-14523.
- A Ibaqumi M. et al.; KCa3. 1 potassium channels are critical for cAMP-dependent chloride secretion and cyst growth in autoeomal-dominant polyeystic kidney disease. Kidney Int. 2008, 74(6):740-749.
- Catacuzzeno, et al.; Expression and Role of the Intermediate-Conductance Calcium-Activated Potassium Channel KCa3.1 in Glioblastoma. Journal of Signal Transduction. 2012,1–11.
Inquiry
